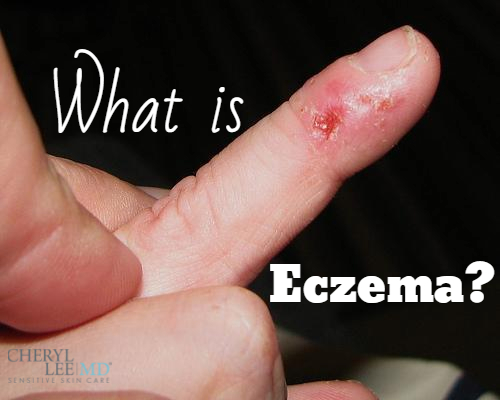
There is nothing worse than being a chronic sufferer from eczema. According to the Bailliére’s Nurses’ Dictionary, eczema can be defined as “a general term for any superficial inflammatory process involving the epidermis primarily, marked early by redness, itching, minute papules and vesicles, weeping, oozing and crusting, and later by scaling, lichenification and often pigmentation.” In other words, it is a blanket term used to describe many dry, skin conditions.
What Causes Eczema?
While there is really no known cause for eczema, there are several factors that appear to contribute to it including: environmental aspects, hereditary predispositions and other irritants. If a parent suffers from an atopic disorder, children are more susceptible in being sufferers themselves. If both parents struggle with atopic conditions, the child’s likelihood of developing eczema is even greater.
Some Environmental Factors Include:
- Hot and Cold Temperatures: excessive sweating, extreme heat and low or high humidity.
- Allergens: dandruff, pet dander, dust mites, molds, pollen and dust.
- Foods: wheat, gluten, dairy products, soy, nuts and seeds.
- Irritants: harsh soaps, detergents, perfumes, shampoos, disinfectants and dyes.
- Topical Irritants: juices from meats, fruits and vegetables; sunflower/olive oil and oats/gluten.
- Mood: Stress is not a direct cause of eczema flares; however, it is known to make symptoms worsen.
- Microbes: certain fungi types, viruses and bacteria such as Staphylococcus aureus (which can be found in the nasal cavity, stressing the importance of not picking your nose)!
- Hormones: this is more relatable for women who experience hormonal changes due to menstrual cycles, pregnancy and menopause.
As if the list of influences were not overwhelming enough, the list of treatment options can be equally staggering. There are numerous ways to treat the condition. Some of these options may only alleviate the symptoms depending on the severity of your disorder.
Treatment and Prevention Techniques and Tips:
- Take colder to lukewarm showers, avoiding hot water and long soaks in baths.
- Avoid harsh soaps with fragrances and other allergenic chemicals.
- Make sure you shampoo your hair with shampoos free of sulfates/sulfites.
- Never rub your skin with your towel, pat your skin dry.
- Moisturize your skin within 3-5 minutes after showering for best absorption and benefits.
- Utilize creams that focus on skin barrier optimization (SBO), contain healing ceramides and are hypoallergenic for moisturizing.
- Use a humidifier in extreme hot and cold weather.
- Keep your fingernails trimmed short to avoid : scratching at your flare-ups, opening wounds and potentially creating a breeding ground for bacteria such as Staphylococcus aureus.
- Learn your eczema triggers. Keeping a daily journal can help you to identify them.
Mild to moderate eczema will likely benefit greatly from the treatment above; however, it may only alleviate symptoms. For chronic sufferers of the condition or those who are having difficulty achieving relief, set up an appointment to speak with a reputable dermatologist to discuss other options available for your treatment regimen.
There is a plethora of medications that your doctor can prescribe for treatment of eczema and other skin disorders including: topical steroid creams, antibiotics, phototherapy, medications for fungla infections and topical calcineurin inhibitors.
Dr, Cheryl Lee Eberting blogs regularly about skin problems, treatment and after care.
